Medical Practice Settles for $600,000 after Violating False Claims Act

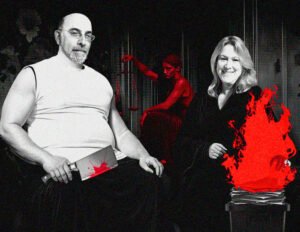
Owners of Orange Medical Care P.C. have settled federal charges that they improperly billed Medicare for rendered services. Promotional photo by Orange Medical Care, retrieved from Google Maps.
The government filed and simultaneously settled the civil lawsuit.
Prosecutors claim Orange Medical committed fraud by billing Medicare and Medicaid by submitting claims for primary care services that were not rendered or supervised by Medicare and Medicaid-enrolled physicians between November 2026 and December 2022. Ashikkumar and Manish Raval own Orange Medical.
Billing for Medicare/Medicaid Services Rendered by Non-Enrolled Physicians
Orange Medical also altered patients’ records claiming that one of the Ravals had seen the patient who another provider saw, according to the settlement agreement between the feds and the Ravals.
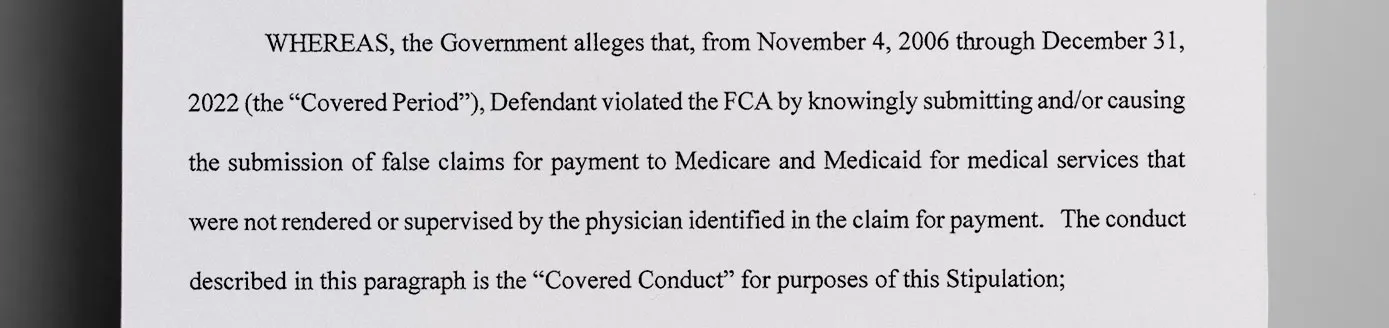
In an e-mail from February 2016, Ashikkumar A. Raval sent instructions to a third-party billing company to seek reimbursement for services provided by non-credentialed providers, stating, “Until all the providers are credentialed… (Orange Medical) will have to bill under the provider who is credentialed. Please do not hold any billing for that reason,” according to their stipulation in court.

The Ravals instructed third-party payment services to bill Medicare under the names of enrolled providers when non-enrolled providers gave the services, according to the government’s case.
In some cases, the Ravals claimed to be attending physicians on Medicare and Medicaid reimbursement claims, even when they were traveling outside of the country at the time and not physically at their practice.
Charges Came on the Heels of a Whistleblower Report
These practices came to light when whistleblower Niki Patel, a former employee who worked for Orange Medical for over a year, filed a false claims complaint, alleging that Ravals violated the federal False Claims Act and the New York False Claims Act. It is unknown why it took over eight years for the investigation to be completed and the settlement between the two parties to be reached.
“As a part of this settlement, the defendants acknowledged that Orange Medical obtained funds from the Medicare and Medicaid programs for claims that did not comply with those programs’ billing rules,” HHS-OIG Special Agent in Charge Naomi Gruchacz said in the press release announcing the settlement. “Individuals and entities that participate in the federal health care system are required to obey the laws meant to preserve the integrity of program funds and the provision of appropriate, quality services to patients.”
Reimbursing Medicare and Medicaid
The Ravals must reimburse $600,000, including $268,800 to pay back Medicare and $331,200 to reimburse New York State, which is the co-administrator of the Medicaid program for low-income individuals, according to the settlement terms.
The Ravals consented to a $1,646,835 judgment, but the government agreed to accept a lowered penalty due to the financial condition that the Ravals were in at the moment of the sentencing. However, court documents state that if the Ravals misrepresent their net worth by $60,000 or more, the United States can reinstate the lawsuit and collect the full $1.6 million settlement.
How to report Medicare or Medicaid fraud?
To report suspected Medicare fraud, call 1-800-HHS-TIPS (1-800-447-8477) or submit a report here. Another option is to visit your local Medicare or Medicaid office and do it in person.
Discover More Muck
First AI-Powered Lawsuit Exposes California’s Eco-Fraud Empire
Feature John Lynn | Apr 10, 2025
Former Child Soldier General Lied to Get Green Card
Report Strahinja Nikolić | Feb 27, 2025

Weekly Muck
Join the mission and subscribe to our newsletter. In exchange, we promise to fight for justice.
Weekly
Muck
Join the mission and subscribe to our newsletter. In exchange, we promise to fight for justice.