UCHealth to Pay $23 Million to Resolve False Claims Act Violations

In a settlement with the federal government, UCHealth will pay $23 million for violating the False Claims Act by allegedly upcoding emergency room visits.
UCHealth will pay $23 million according to the terms of its settlement with the federal government.
This case is unique since UCHealth is partially owned by the State of Colorado. In 2012, the University of Colorado Hospital, a state agency, created UC Health as a joint company with Poudre Valley Health, according to coverage by the Denver Post. UCHealth operates as a not-for-profit medical service provider and is headquartered in Aurora, Colo.
UCHealth did not admit to wrongdoing in agreeing to the settlement.
Whistleblower Brought Problem to Light
A sizeable chunk– $3.91 million– of the settlement will go to Timothy Sanders under the whistleblower provisions of the False Claims Act, according to the press release. These provisions allow for people who report fraud to be eligible for part of the money recovered by the federal government in cases like this.
Sanders had pointed out the irregularities while working as a revenue recovery auditor for UCHealth and dealt with complaints from patients who felt they were overcharged. During the trial, Sanders said that the automated billing system was overcharging people and that several people on his team, as well as UCHealth’s Chief Financial Officer at the time, knew about it.
Sanders also claimed that he resolved 64 cases from patients billed as level 5 emergency room visits. Seven were bumped down to a level 2 visit, 29 were changed to a level 3 and 28 were reduced to level 4.
What is Upcoding?
Medical billing “upcoding” happens when providers use codes for more severe (and expensive) services than are warranted by patients’ conditions, according to a 2021 article posted on the NIH website.
Federal programs, such as Tricare and Medicare, are often targeted in upcoded claims. Federal authorities consider intentional upcoding a kind of fraud and prosecute medical providers they believe engage in the practice, as they did in this case with UCHealth.
Automatic Upcoding of ER Visits
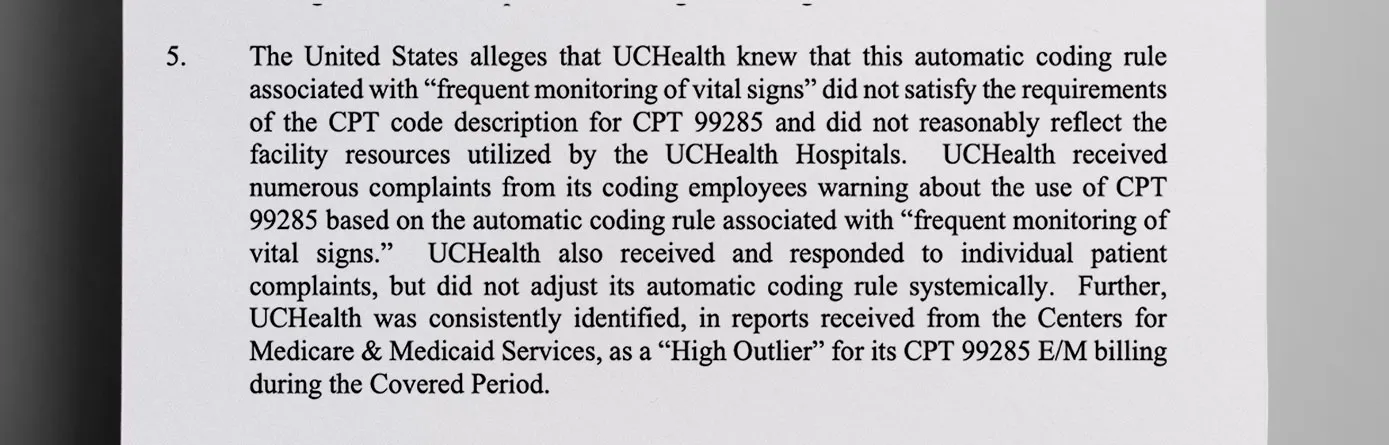
The crux of the federal case against UCHealth was allegations that from November 1, 2017, through March 31, 2021, UCHealth hospitals automatically coded certain claims for emergency room visits using CPT 99285, according to a summary of the federal charges in the settlement.
This code– CPT 99285– is supposed to be reserved for the most serious cases and means that UCHealth frequently checked vital signs, more than once an hour for the duration the patient was in the ER. The problem was they did this in cases that did not merit it, so they checked vital signs frequently and overcharged individuals and federal programs for it, according to claims in court documents.
Federal authorities alleged that UCHealth leaders were aware that the automatic coding rule associated with monitoring vital signs did not satisfy the requirements for billing to Medicare and TRICARE because it did not reasonably reflect the facility resources used by the UCHealth hospitals.
It wasn’t just federal programs affected by this automatic upcoding. Patients also paid higher out-of-pocket expenses due to the practice, according to several billing disputes presented to the court.
Comments by Officials
Officials involved in the case noted that upcoding may enrich medical providers, but they do so at the cost of programs individuals rely on for health care.
Acting U. S. Attorney Matt Kirsch said, “Fraudulent billing by healthcare companies undermines Medicare and other federal healthcare programs that are vital to many Coloradans.”
“We will hold accountable health care companies who adopt automatic coding practices that lead to unnecessary and improper billing,” Kirsch said.
UCHealth Denies Wrongdoing
CBS News shared a UCHealth statement about all the cases in which they denied wrongdoing.
“UCHealth is pleased to see the end of this lengthy and resource-intensive investigation. UCHealth denies these allegations, but we agreed to the settlement to avoid potentially lengthy and costly litigation. The settlement allows us to focus our resources on providing excellent patient care,” the statement said.
Other Recent Health Care Fraud Cases
This is not the only recent Medicare fraud case covered by The Daily Muck.
In March 2024, Robert M. Clark of Florida pled guilty to charges related to his role in bilking Medicare for more than $30 million, while John M. Spivey, a 53-year-old man from New Orleans, pled guilty to one count of conspiracy in connection with a scheme to bill for medically unnecessary cancer and cardiovascular genetic testing.
Discover More Muck
First AI-Powered Lawsuit Exposes California’s Eco-Fraud Empire
Feature John Lynn | Apr 10, 2025
Former Child Soldier General Lied to Get Green Card
Report Strahinja Nikolić | Feb 27, 2025

Weekly Muck
Join the mission and subscribe to our newsletter. In exchange, we promise to fight for justice.
Weekly
Muck
Join the mission and subscribe to our newsletter. In exchange, we promise to fight for justice.