Walgreens to Pay More than $100 Million to Settle Claims of Billing Government for Undispensed Prescriptions

Walgreens has agreed to pay more than $100 for billing the government for undispensed subscriptions. Photo credit: Elliott Cowand Jr / Shutterstock.com.
Walgreens has agreed to a settlement of $106.8 million for allegedly billing government healthcare programs for prescriptions that they never filled, according to a Sept. 13 DOJ press release. These acts violated the False Claims Act and other state statutes.
Based in Deerfield, Illinois, Walgreens, one of the country’s largest retail pharmacy chains, allegedly submitted false claims from 2009 to 2020 for prescriptions that were processed as being claimed but were never retrieved by the patient, as detailed in the press release. They made claims to Medicare, Medicaid, and other healthcare programs with federal funding. As a result, the company received millions of dollars for prescriptions they never filled or gave to the beneficiaries of the health care programs.
Multiple Qui Tam Lawsuits
The $106.8 million will settle multiple qui tam actions that were filed against Walgreens, according to the press release. A qui tam action is a person, or “relator,” who sues or brings action against a company or individual on the government’s behalf. If the government wins the suit, the relator receives a portion of the award. Relators can receive up to 30% of the government’s settlement in qui tam actions in False Claims Act lawsuits.
Bustos Lawsuit Against Walgreens
On Sept. 3, 2015, Andrew Bustos filed a qui tam action against Walgreens, alleging that the company submitted false claims to the Medicare Part B Program between January 2009 and December 2015 for medical equipment, prescription medications, and other related supplies that were never given to their customers, according to the Bustos settlement. Walgreens is to pay $9 million in the settlement but maintains that it is not an admission of guilt.
The United States will pay Bustos $1.6 million, according to the settlement.
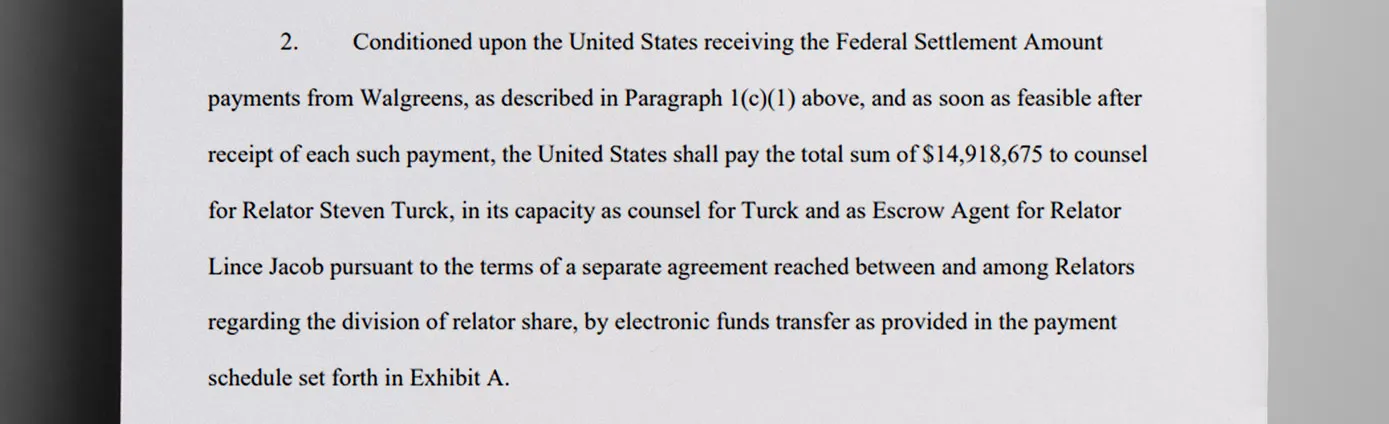
Turck and Jacob Lawsuits Against Walgreens
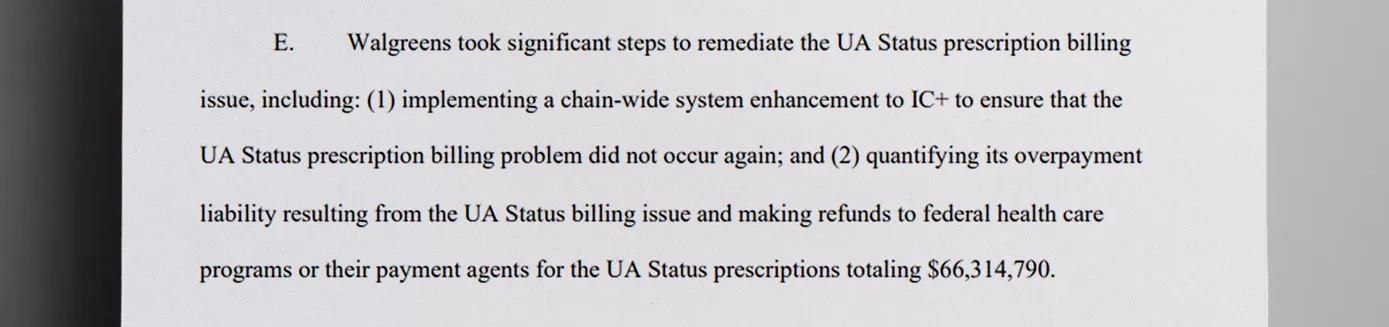
On April 26, 2019, Steven Turck filed a qui tam action against Walgreens, and on April 23, 2020, Lince Jacob did the same, according to the Jacob settlement. After the first filing, under an agreement between Walgreens and the Office of Inspector General at the Health and Human Services, Walgreens disclosed issues with its billing system that caused it to bill federal health care programs for prescriptions patients didn’t receive.
Prescriptions Not Dispensed
In the lawsuits, the government maintained that `Walgreens used the Intercom Plus pharmacy management system, according to the Jacob settlement. The prescriptions were processed through this system but not dispensed or delivered in 30 days. Walgreens cooperated with the investigation and refunded $66,314,790, so they will receive a credit for that amount in the final judgment.
Crackdown on Healthcare Fraud
The DOJ announced a nationwide healthcare fraud enforcement action in a press conference on June 27. Criminal charges against 193 defendants and millions of dollars recovered have resulted from going after companies that take advantage of the system.
“This settlement marks another major achievement in our ongoing commitment to combat healthcare fraud,” U.S. Attorney Roger B. Handberg for the Middle District of Florida said, speaking about the $106.8 million settlement in the DOJ release.
Discover More Muck
First AI-Powered Lawsuit Exposes California’s Eco-Fraud Empire
Feature John Lynn | Apr 10, 2025
Weekly Muck
Join the mission and subscribe to our newsletter. In exchange, we promise to fight for justice.
Weekly
Muck
Join the mission and subscribe to our newsletter. In exchange, we promise to fight for justice.