Forced Labor: The Industrialization of Birth
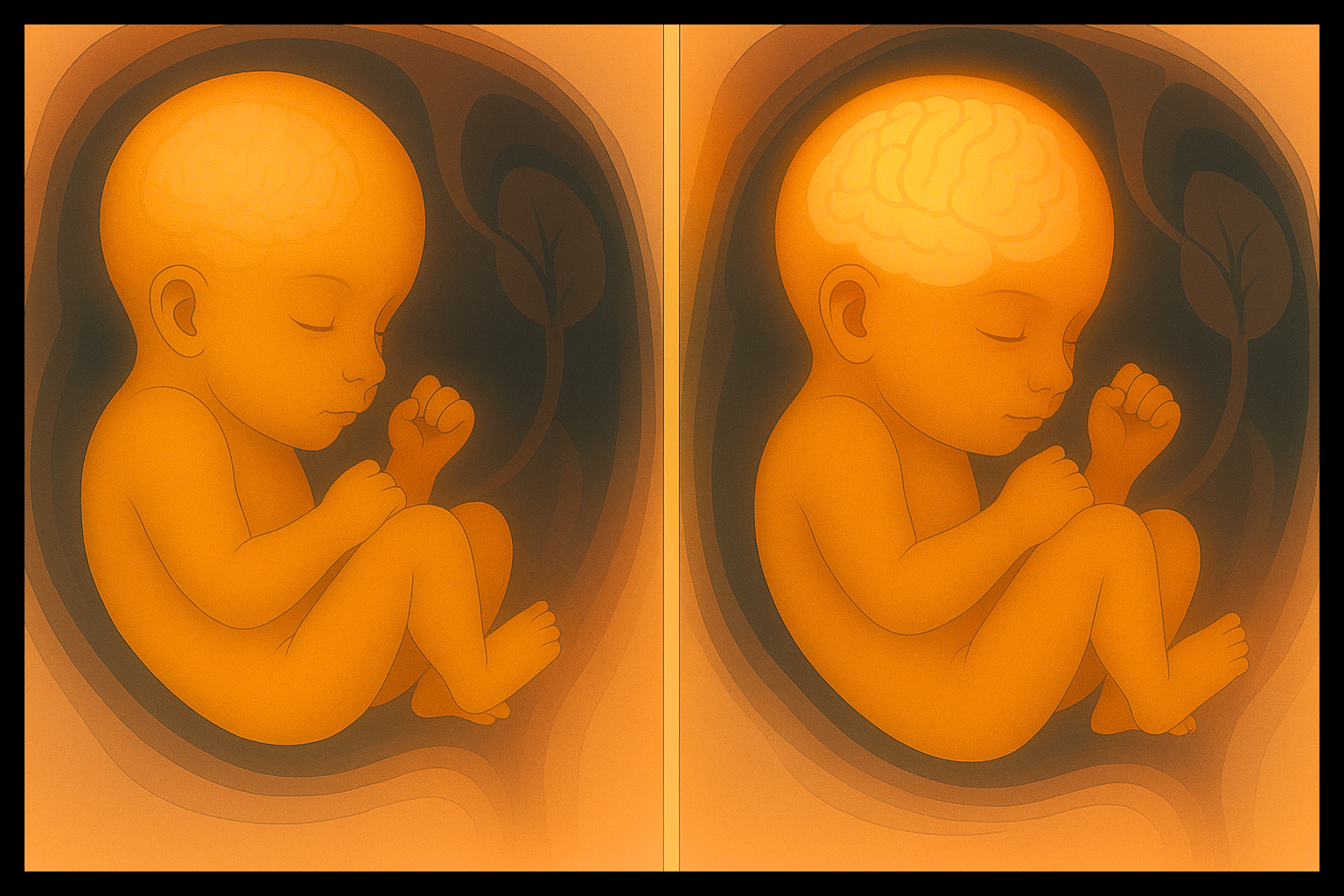
At 35 weeks, a baby’s brain is just two-thirds the size it will be at full term. Those final weeks aren’t extra—they’re essential. Lungs mature. Immunity strengthens. The brain nearly doubles in weight.
Yet, too many babies are born early—not because of medical necessity, but because hospital systems prioritize efficiency over development.
In the U.S., more than 1 in 3 births are artificially induced, often scheduled before labor begins naturally. Women are told when to give birth, not based on their body’s signals, but on a hospital’s calendar.
Why? Inductions are easier to staff, simpler to manage, and often more profitable—especially when they lead to C-sections or neonatal intensive care (NICU) stays.
This isn’t about safety. It’s about control. And the consequences are clear: more trauma, more surgery, more babies delivered early—not by nature, but by design.
The Quiet Pressure to Induce
For many women, the choice to induce labor feels like no choice at all.
In a Scary Mommy essay, a first-time mother recalls being five days past her Christmas due date when her OB/GYN asked if she wanted to be induced. It was, as she put it, “barely the first time I’d heard the word, let alone considered the decision.” No risks were explained. No options were offered. The doctor simply raised her eyebrows and waited.
When she hesitated—“You mean, like, now?”—the OB said yes, adding that otherwise she’d likely have to wait until January due to holiday staffing.
The pressure was unspoken but palpable. “Her body language was impatient, and I didn’t feel like I should ask any questions, given the tension in the room, and my excitement to meet my first child,” she wrote. “So I said yes.”
Years later, with four kids and a hard-earned perspective, she looks back on that moment with clarity and frustration: “As a first-time mom, this should have been at least a 20-minute discussion, possibly with an overnight period to think about it… Now, I know more.”
For some, the stakes are devastating. Monica Cerna, featured in a recent Daily Muck investigation, faced similar pressure.
At 39 weeks, her doctors recommended induction without explaining the procedure or risks, including the use of Pitocin to trigger contractions. “They weren’t telling me what was going on as much as they should have,” Cerna testified.
Hours of intense, drug-induced contractions led to an emergency C-section and permanent brain injury to her daughter, who now lives with cerebral palsy.
These stories aren’t outliers. Nearly 40% of all inductions in the U.S. are elective, meaning they’re scheduled out of convenience. That’s close to half a million babies born each year without a clear medical reason.
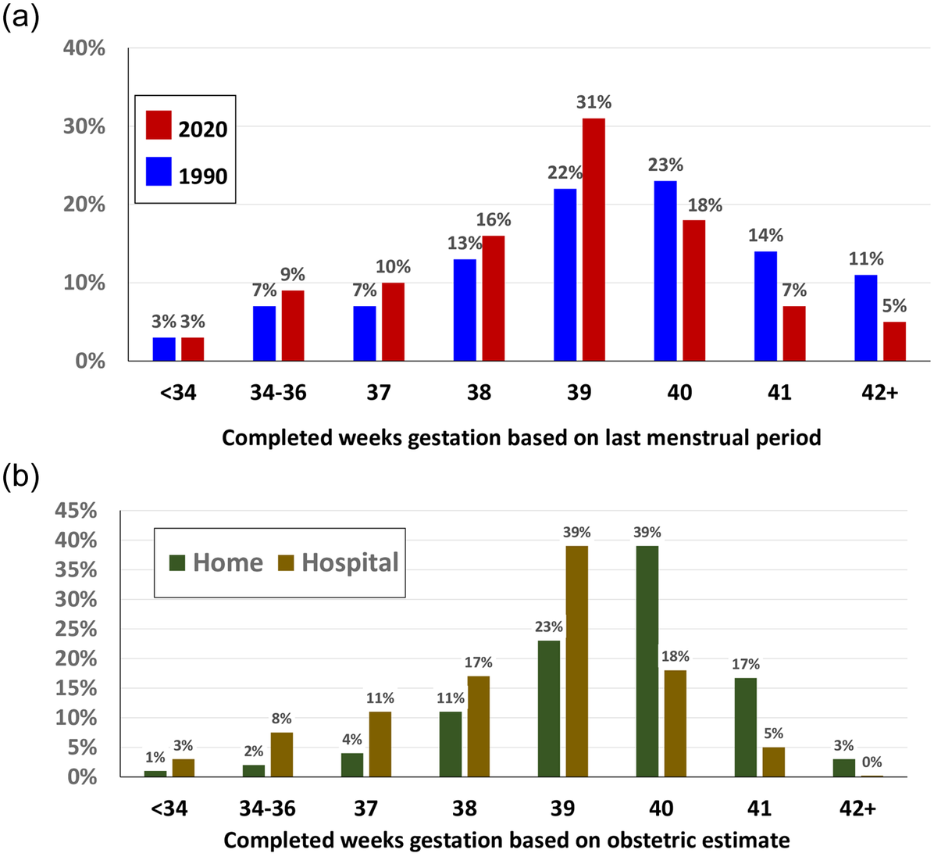
(a) From 1990 to 2020, the percentage of births occurring at 40 weeks dropped by nearly half, while 39 weeks became the new peak—coinciding with increased labor induction rates.
(b) In 2020, home births still peaked at 40 weeks, while hospital births clustered earlier, at 39 weeks or below—highlighting how institutional settings disrupt natural gestation timelines.
Source: National Vital Statistics System (NVSS), 1990 & 2020 Public Use Datasets. Reproduced from Declercq et al. (2023), PLOS ONE, https://doi.org/10.1371/journal.pone.0278856
The Harm Is Real
Inducing labor without medical need disrupts the body’s natural timeline–and the consequences can be life-altering. Mothers are pulled into a chain of unnecessary interventions. Babies are denied the final days and weeks of growth they need most.
Risks to Mothers
For first-time mothers, elective induction nearly doubles the chance of a C-section, a major surgery with longer recovery and higher risk of complications. For women with C-sections, induction triples the risk of uterine rupture—a rare but life-threatening emergency.
The process itself is grueling. Induced contractions, driven by drugs like Pitocin, are longer, stronger, and more painful, increasing the odds of postpartum hemorrhage—severe bleeding after birth—by 56%.
Beyond the physical pain, induction often means IVs, monitors, and restricted movement, turning birth into a clinical ordeal that on average lasts hours longer than natural births.
A Swedish study found that women with induced labor were 60% more likely to report negative birth experiences, which can increase the risk of postpartum depression, particularly when combined with cesarean sections or infant complications
Risks to Babies
And for the baby, the risks are more stark—and in some cases, longer-lasting.

Interrupting the baby’s brain development in the final weeks of pregnancy means cutting short the most critical phase of neurological growth. These aren’t finishing touches—they’re foundational circuits for memory, learning, and emotional regulation.
Inducing labor early doesn’t just move up the timeline—it cuts the brain-building process short.
And here’s what almost no one tells expecting parents: about 1 in 4 naturally-timed births occur after 41 weeks. So when a baby is electively delivered at 39, they may be arriving up to two weeks early.
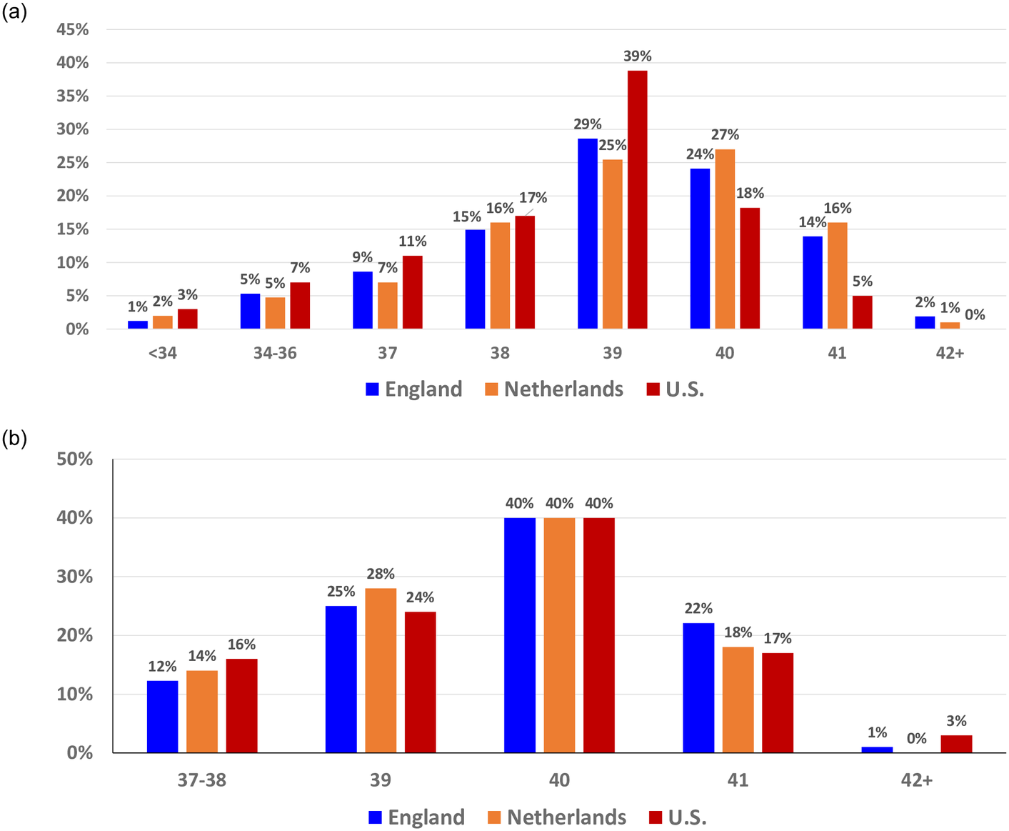
(a) In 2020, 76% of U.S. births occurred before 40 weeks, versus just 60% in England and 56% in the Netherlands.
(b) Yet when births occur at home—outside hospital systems—all three countries show an identical peak at 40 weeks, reinforcing that the natural timing of birth is consistent globally and only disrupted by hospital protocols.
Sources: CDC Wonder (U.S.), Office for National Statistics (England), Peristat.nl (Netherlands). Reproduced from Declercq et al. (2023), PLOS ONE, https://doi.org/10.1371/journal.pone.0278856
A neonatal outcomes study showed babies born slightly early (34–38 weeks) are up to 45% more likely to require NICU admission, often for respiratory distress, jaundice, or feeding difficulties. They also face higher rates of breastfeeding problems and hospital readmissions.
But the consequences don’t always end in the hospital. Research now links early-term, provider-initiated births to long-term developmental concerns. These include increased risks of learning delays, language impairment, and attention problems—issues that may not emerge until school age.
The Cost of Cutting Corners
When hospitals prioritize schedules over health, the price isn’t just paid in pain—it’s billed to families and taxpayers, dollar by devastating dollar.
Inductions that spiral into complications—like C-sections or neonatal intensive care (NICU) stays—carry a steep cost. A cesarean birth, often triggered by failed inductions, on average costs $4,000 more than a vaginal delivery due to surgery, anesthesia, and longer hospital stays.
For newborns, even slightly early births can mean NICU bills that typically exceed $3,500 per day—not for emergencies, but for avoidable interventions.
These aren’t just numbers. They’re families facing crushing co-pays, missed work, and the trauma of watching a newborn struggle in intensive care.
Hospitals can break this cycle, and some have. At Seton Hospital in Texas, banning elective inductions before 39 weeks slashed costs related to birth trauma from $4.5 million to $180,000 in one year. Fewer babies needed intensive care. Fewer mothers faced surgical recoveries. The savings reflected healthier outcomes, not just smaller budgets.
State and national programs prove this isn’t a fluke.
Texas led the way in 2011, with Medicaid reforms that ended coverage for early elective deliveries. Inductions fell 14%, babies were born healthier, and more states followed.
The federal Strong Start initiative expanded this momentum nationwide, targeting Medicaid-funded births to reduce early elective deliveries. Between 2012 and 2017, it helped drive non-medically necessary inductions before 39 weeks down from 17% to under 2%. Birth center care alone cut preterm births by nearly a third and saved Medicaid an average of $2,000 per delivery. By avoiding costly complications like NICU stays and C-sections, Strong Start proved that better timing leads to better outcomes—and real savings for families and taxpayers alike.
But the path forward is far from over, and these initiatives are isolated in scope and geography. National and state movements are required to ensure no mother is coerced into giving uninformed consent.
The System That Keeps Pushing
Elective induction remains widespread not because it’s safer—but because the system is structured to encourage it.
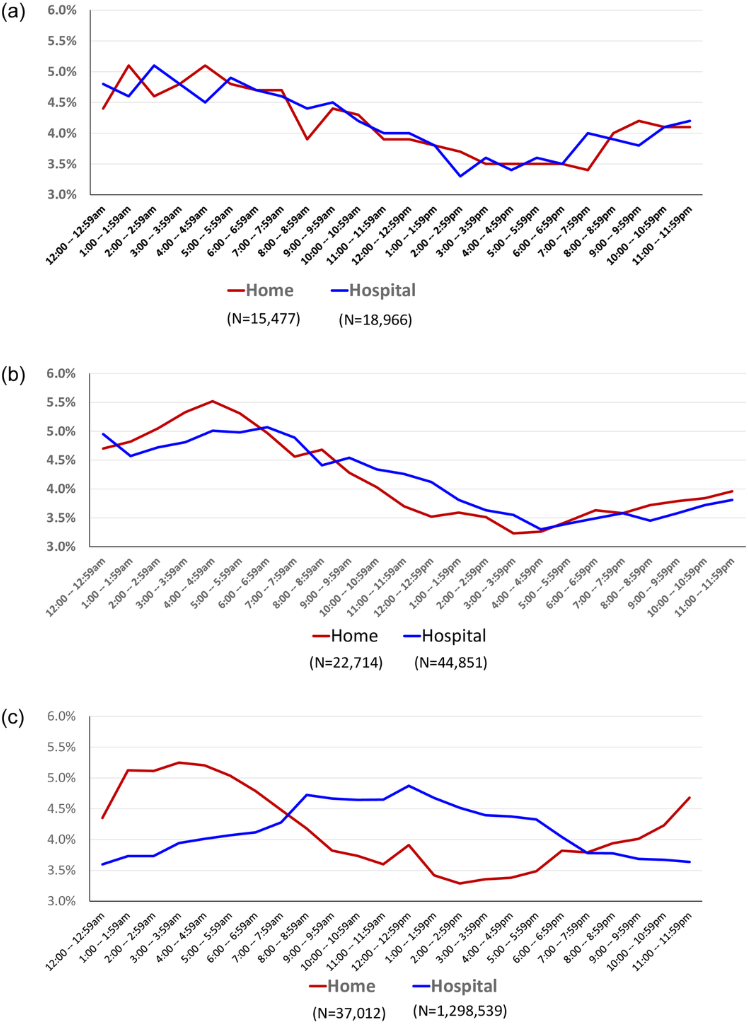
(a–b) In England and the Netherlands, hospital births without intervention follow the same early-morning pattern as home births, suggesting alignment with natural labor rhythms.
(c) In the U.S., the pattern is inverted: hospital births without induction or augmentation peak during standard business hours (8 a.m.–5 p.m.), indicating systemic scheduling influence even when intervention is not formally recorded.
Source: National Vital Statistics System (U.S.); Birthplace Study (England); Peristat.nl (Netherlands). Reproduced from Declercq et al. (2023), PLOS ONE, https://doi.org/10.1371/journal.pone.0278856
Hospitals benefit operationally and financially from scheduled deliveries. Planned inductions allow for efficient staffing, fewer emergency calls, and higher billing rates through layered interventions: drugs, monitoring, and frequently, C-sections.
Fueling this trend, the ARRIVE Trial has been misused to justify routine elective inductions despite significant flaws including design issues, biases, and real-world dangers.
Doctors and hospitals aren’t just responding to money. They’re also responding to fear.
Obstetrics is one of the most heavily litigated fields in medicine. Providers know that if something goes wrong—a stillbirth at 41 weeks, a difficult delivery—they may face a lawsuit, even if they followed best practices of not inducing. So many choose to act early, not because it’s necessary, but because it feels safer. There is a natural human bias towards doing something over nothing.
Consent Without Clarity
Every medical procedure requires informed consent—but when it comes to elective labor induction, that consent is often given without real information, context, or choice.
They’re told their baby might be too big, or that they’re “overdue” at 39 weeks, or that induction is safer. Rarely are they told it can double the risk of a C-section, stall labor, increase bleeding, or land their baby in the NICU.
Most women don’t know the risks because they’ve been misinformed. A national survey revealed:
- 75% of women mistakenly believed that “full term” meant before 39 weeks—despite medical guidelines defining full term as 39 to 40 weeks.
- Over 90% thought it was safe to deliver early even when there was no medical reason to do so—reflecting widespread confusion about the risks of elective early delivery.
These aren’t minor misunderstandings. They’re foundational errors that make real informed consent impossible. When women don’t have the facts, the choice isn’t truly theirs.
And pressure is common. One in four women who were induced said they felt pressured by their provider—three times the rate of those who weren’t.
Too often, consent is just a box to check, not a safeguard. Real informed consent starts with facts—delivered clearly, before any decision is made—not after a path has already been pushed.
A Law That Costs Nothing—And Changes Everything
This crisis doesn’t require billions. It needs two simple reforms: real informed consent and radical transparency. The Daily Muck is spearheading a movement to bring about a bill to establish just that.
1. Mandatory Waiver for Elective Inductions
Such a bill would require that labor inductions, performed before 40 weeks and without a medically indicated reason, cannot be scheduled without the following.
Your doctor must provide and read out loud a waiver with these facts:
- Brain Development: A baby’s brain at 35 weeks weighs only about two-thirds of its weight at 39–40 weeks (NIH). Early induction would cut short this critical period of brain growth.
- Due Dates Are Estimates: Only about 5% of babies are born on their exact due date. Many healthy pregnancies go past 40 weeks. 41–42 weeks is still within the normal range (ACOG).
- Hormonal Readiness: Natural labor triggers hormones that help the baby breathe and protect the brain. Adrenaline clears lung fluid; oxytocin reduces oxygen needs. Inducing early may bypass these protections, raising risks of NICU admission (PMC).
2. Demand Hospital Accountability
Most patients have no idea how often their hospital induces labor—or why.
That needs to change.
The Daily Muck is calling for a public reporting mandate requiring every hospital to publish its rate of labor induction—broken down by gestational age, medical vs. non-medical reasons, and first-time vs. repeat births.
If a hospital is routinely inducing before 39 or 40 weeks without medical necessity, the public deserves to know.
When hospitals know they’ll be held accountable, they think twice about pushing convenience over care.
What You Can Do
Hundreds of thousands of babies are born too soon each year—not to save lives, but to fit hospital schedules.
If you believe mothers deserve truth—and babies deserve time to grow—here’s how you can help:
-
-
- Share the Truth: Spread this article on social media, email, or in person. Most people don’t know hospitals prioritize efficiency over health. Break the silence.
- Stay Informed: Subscribe to The Daily Muck for updates on our investigations, new legislation, and ways to act. Knowledge is power—join us.
- Demand Change: Call or email your state representatives. Urge them to support laws requiring honest consent and hospital transparency for inductions. Visit congress.gov for contact info. The Daily Muck is drafting model legislation—tell lawmakers you back it.
- Amplify the Fight: Follow us on X (@TheDailyMuck). Every retweet, every voice, builds momentum to hold hospitals accountable.
At The Daily Muck, we follow the money, the silence, and the harm—wherever it leads. This story isn’t over.
-
Discover More Muck
Dead on ARRIVAL: Fatal flaws in the ARRIVE Trial and Hidden Dangers of Elective Inductions
Feature John Lynn | Sep 15, 2025

Prioritizing Rural Births: Senator Casey Murdock on Enhancing Maternal Care
Report John Lynn | Aug 28, 2025

Advancing Access: Senator Becky Massey on Maternal Health Reforms
Report John Lynn | Aug 18, 2025

Weekly Muck
Join the mission and subscribe to our newsletter. In exchange, we promise to fight for justice.
Weekly
Muck
Join the mission and subscribe to our newsletter. In exchange, we promise to fight for justice.